1801006129 long case
march 17,2023.TH A
79 Y/O MALE WITH RECURRENT CVA AND LEFT HEMIPLEGIA WITH ASPIRATION PNEUMONIA AND SEIZURES DISORDER.
CHEIF COMPLAINTS :-
A 79 year old male was brought to the OPD with cheif complaints:
.C/o altered sensorium since 5 days.
. fever since 10 days
.complaints of cough since 20 days
. difficulty in swallowing since 1 month.
HOPI :-
Patient was apparently asymptomatic 20days back then he developed cough which was insidious in onset and gradually progressive. The cough was productive but patient was not able to spit it out and he also faced Difficulty in swallowing.
20 days back ( on feb 25th) he started to have cough and cold
H/o change of voice since 20 days, insidious, hoarse in character and
Slurring of speech was seen.
H/o cough on intake of liquids.
No h/o hemoptysis, difficulty in breathing, breathlessness.
High grade Fever was since 10 days associated with Chills and rigours
There is no history of vomiting, chest pain, loose stools.
PAST HISTORY
Patient is a k/c/o Hypertension and type 2 diabetes since past 10years for which he is on medications I.e tab TELMA AM 40mg po/od. Tab zoryl mv , po/od
K/c/o CVA with left hemiplegia since 7 years.
K/c/o hypothyroidism since 5 years
K/c/o seizures disorder since 2 years
. 10 years back , patient developed lesions on his both foot and out of no where and went to the doctor and found to have diabetes and was put on medication and after 1 year with regular check up he was diagnosed Hypertension and was put on antihypertensive medication.
.7 years back, patient developed head ache at morning, shoulder ache at evening and become sick by night followed by vomtings he was taken to the hospital, but on that night itself he developed left hand pain and itching
Patient was awake on that night due to left hand weakness and itching
-On NEXT DAY Morning they took him to hospital And the Patient was able to lift his hand But was unable to hold objects.
. AFTER 3 DAYS patient developed left sided hemiplegia.
An MRI report was taken and it showed 3 infarcts.
Patient stayed for one and half month in hospital and there was no improvement and so got discharged.
He took liquid deit for 3 months because the patient was unable to eat solid foods and then he slowly started eating solid foods.
patient has 2 attacks of Covid.
-> AFTER 3 YEARS [2020] He had Cough for 2days With Fever on 2nd day and was Diagnosed with covid this was the first time he got COVID for and it resolved
-> AFTER 1 YEAR [2021] He was Diagnosed with COVID for 2nd time and got it resolved.
after covid
.From 7 years onwards , patient was bedridden with foleys attached to him and physiotherapy was done by his attenders daily, but there no improvement was seen
. 20 days back, from March 1st onwards patient developed slurring of speech, mild cough unable to clear the throat secretions and decreased responsiveness and was taken to the hospital and was treated with antibiotics and patient was brought here for further evaluation.
DRUG HISTORY:
.Tab TELMA AM 40mg po/od since past 10years
.Tab zoryl mv , po/od
.Tab levipil 500mg since 2 years
.thyronorm 25mcg. Since5 years
PERSONAL HISTORY :-
Appetite - decreased
diet - mixed
Bowel- Constipated
Bladder - regular
No known allergies and Addictions
Family History- not significant
GENERAL EXAMINATION :-
O/e PT IS arousable but not oriented. Pt not cooperative mostly.
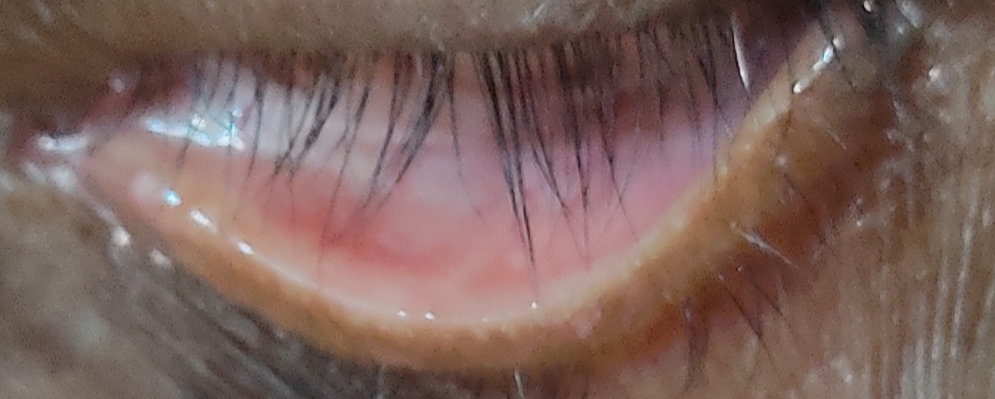
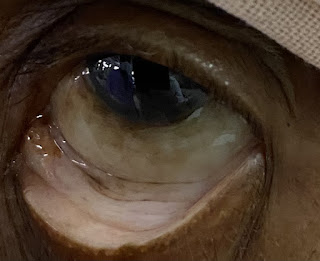
. pallor: PRESENT
. no pedal edema, icterus, cyanosis, clubbing, lymphadenopathy
Respiratory:
CNS EXAMINATION:
GCS( Glasgow coma scale)
CRANIAL NERVES Examination:
1. CN1:
Sence of Smell - Normal
2. CN2:
visual acuity - decreased on left side
3. 3,4,6 CN
EOM movement - could not perform
Pupil size - 2, 3 mmDirect light reflex/consensual light reflex/accommodation reflex - present, present
Ptosis - absent, absent
Nystagmus - absent, absent
Sensory over face & buccal mucosa - N, N
Motor - masseter, Temporalis, pterigoids - N, N
Reflexes - Corneal,Conjunctival - N, N
7 CN
Motor
Nasolabial fold - equal om both sides
Occipito frontalis - equal om both sides
Orbicularis oculi - equal om both sides
Orbicular oris - equal om both sides
Buccinator - equal om both sides
Sensory:
Taste over anterior two third of tongue - cant be performed
MOTOR SYSTEM EXAMINATION :- could not be performed
Power - could not be performed
U/L ->
Superficial reflexes -
Corneal - N, N
Conjunctival - N, N
Abdominal - N, N
DEEP TENDON RELEXES:
Cerebellar examination - could not be performed
Finger Nose test
Finger finger test
Dysdiadokinesia
Heel knee test
Tandem walking
Dysmetria
Intention tremor
Rebound phenomenon
Nystagmus
Titubation
Rhombergs test
SIGNS OF MENINGEAL IRRITATION: absent
Sensory System examination - could not be performed
Crude touch
Pain
Temperature
Posterior Column
fine touch
Vibration
position sense
Cortical -
Two point discrimination
Tactile localization
Graphesthesia
Stereognosis
Gait could not be done
Examination of other Systems - NAD +
CVS :-
Auscultation: s1s2 +,no murmurs
P/A :-
inspection: umbilicus is central and inverted, all quadrants moving equally with respiration,no scars,sinuses, engorged veins, pulsations
auscultation: no bowel sounds heard
bed sores
C/o asymptomatic lesions all over the body since 2 months
H/o application of unknown topical medications used
On examination, multiple hyperpigmented lesions were seen all over the body with scaly lesions over the upper back
Diffuse xerosis present
single ulcer of size 1.5x1.5 cm over the back.
Diagnosis - Senile Xerosis with post inflammatory hyperpigmentation.
A pressure ulcer was also seen at base of scrotum
INVESTIGATIONS:
HbsAg rapid - negative
Xray -
Blood urea -30mg/dl
HBA1C-6.7%
HIV 1/2 RAPID TEST - NON REACTIVE
Anti HCV antibodies rapid - nonreactive
TOTAL BILIRUBIN -0.81mg/dl(normal-0 to 1mg/dl)
Direct bilirubin-0.17mg/dl(0 to 0.2mg /dl)
Serum creatinine -0.9 mg/dl (0.8 to 1.3 mg /dl)
Electrolytes -
Sodium 135meq/l
Potassium 3.5 meq/l
Chloride 98meq/l
Calcium -1.06 mmol/l
PROVISIONAL DIAGNOSIS:-
Recurrent CVA with T2 DM, hypertension with seizures disorder.
TREATMENT:-
1) TAB ECOSPRIN 150 mg RT/OD
2) TAB CLOPIDOGREL 75 MG RT/OD
3) TAB ATORVAS 20 MG RT/OD
4) NEBULISATION - 3% NS ,
MUCUMZY 8th hourly
5) CHEST PHYSIOTHERAPY.
6) RT FEEDS 100 ML WATER 2nd HRLY
50 ML Milk 2nd HRLY.
8) TAB. THYRONORM 25MCG RT/OD
9) TAB. LEVIPiL








COMMENTS