A 24 year old patient with history of vomiting
JANUARY 6th,2023
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 24 year old male who is a resident of Nalgonda and band worker by occupation came with (31.12.22)
CHIEF COMPLAINTS:
.Vomiting since 10 days
.shortness of breath since 10 days
.Difficulty in swallowing and oral ulcers since 9 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10 days back then he developed severe vomitings due to an excessive drinking of alcohol without any consumption of food. The vomitings were 4-5 episodes/day and were non bilious, non blood stained, non foul smelling, watery and occurred immediately after consumption of food or liquids. Also complaints of difficulty in swallowing since 9 days.
Patient developed oral ulcerations later that day. He was taken to a local hospital where medication (mouth wash and some gel for ulcers). was provided and did not get relief. 6 days ago he had complaints of shortness of breath (Grade 3) and decreased urine output with blood in the urine. Then went to a private hospital and endoscopy was advised and blood tests were done in which increased serum creatinine levels and bilirubin levels were detected and referred to our hospital and got admitted for dialysis. 5 days ago the patient was observed to develop a white coating in the mouth and over the tongue.
He has no H/o fever, loose stools, pedal oedema, pain abdomen, burning micturition, cold, cough .
PAST HISTORY:
No similar complaints in the past
No H/o HTN, diabetes, asthma, epilepsy and tuberculosis.
PERSONAL HISTORY:
Diet: mixed. Appetite: reduced
Bowel and bladder: irregular.
Sleep: adequate.
Addictions : alcohol consumption since 4 yrs daily( around 180 ml) (excessive drinking episode 2 days back before onset of present symptoms ) and paan occassionally.
Allergies: none.
Family history:
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative moderately built and nourished
Vitals
Temperature: afebrile. PR: 83bpm
RR: 22cpm. BP: 140/90mmHg
Pallor :absent
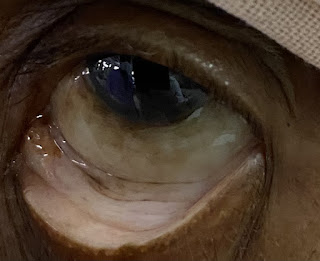
Icterus: present.
Clubbing: absent
Lymphadenopathy: absent
Oedema : absent
SYSTEMIC EXAMINATION:
Per abdomen:
soft on palpation, bowel sounds heard, no distention present.
Respiratory system: no wheeze heard, no crepitus heard, normal vesicular breath sounds heard
CVS: S1 S2 heard, no additional murmurs
CNS: no focal neurological deficits
provisional diagnosis:
INVESTIGATIONS:
CT of thorax
Chest x ray findings
HRCT of thorax :
BLOOD UREA
USG REPORT
Anti HCV ANTIBODIES
HBsAg
HIV TEST
Urine for ketone bodies
Serum iron
Serum electrolytes
Serum Creatinine






























Comments
Post a Comment