A 65 YEAR OLD MALE WITH DECREASED MOVEMENT AND APPETITE.
This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and comprehending clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHEIF COMPLAINTS
A 65 YEAR old male gold craftsmen by occupation who is a resident of Nalgonda was brought to causality with complaints of:
- Improper gait since 2 year.
- Unable to walk properly since 1 year.
- Stiffness of limbs since 15 days.
- Weakness of both limbs since 15 days.
- Decreased appetite since 15 days.
- Unresponsiveness since 4 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 year back then he developed unbalanced gait that was insidious in onset and visited a hospital, patient was said to be normal and discharged.
Since then in the course of 1 year patient was having generalised weakness that was intermittent in nature, not associated with sob.
Patient also had fear of falling down sensation and pricking sensation over the sole since 6 months.
Due to generalised weakness and fear of falling down in the limbs patient was not able to walk properly and was using support of things to walk. Later he was not able to walk at all and stopped walking completely and was bedridden since 2 months.
after this the patient visited a hospital and was advised to take an MRI. In the MRI following where seen:
1. Hydrocephalus
2. Early Parkinson's changes.
2 months back he used to eat by himself and was able to do daily activities like putting on his clothes, take a bath etc, but since one month he was doing all activities with the help of his wife.
2 months ago he also developed sores on both his hips due to pressure while laying down on his sides, more while wearing diapers ( put on by his wife when going out ), so they stopped wearing diapers and the wife rolled him frequently from side to side but the sores still persisted.
patient also suffered from enteric fever 20 days ago and his condition deteriorated further.
since 15 days he had stiffness of his left upper and lower limb, for which his wife rubbed oil and massages which relieved the symptoms a little.
Since 10 days he was not responding to commands and had decreased appetite.
5 days ago he stopped feeding orally and is only kept on IV fluids.
since 3 days PATIENT developed fever which was of high grade not associated with chills is seen, relieved on taking medication.
on 5.12.22
patient came to opd with altered sensorium.
PAST HISTORY:
PATIENT is a know case of hypertension (drug unknown) since 5 years,
He is also a known case of diabetes since 3 years. and was taking glimipiride 2 mg+metformin 500mg.
No history of epilepsy, thyroid, asthma , or any previous surgery.
Personal history -
Mixed diet
Appetite - decreased
Regular bowl and bladder movement
Addiction -alcoholic since 35 yrs used to drink 250 ml everyday.
No allergies.
Family history -
GENERAL EXAMINATION:
Bp - 110/80 mmHg
PR - 96 bpm normal rhythm and volume.
RR - 22
Temp - afebrile
Pallor - present.
Icterus - absent
Clubbing - absent
Lymphadenopathy - absent
Edema - absent
Patient looks dehydrated
Systemic examination:
Respiratory system:
Bilateral air entry present, normal vesicular breath sound heard, trachea is central on palpation.
Cardio vascular system : S1 , S2 heard and no murmurs detectedPer Abdominal examination : Soft and non tender.
Central Nervous system examination:
Higher mental functioning: Patient is conciouss ,non coherent and not oriented to time place and person .
Right handed.
Language : Speech - Aphasic - unable to speak.
Unable to read and write.
Sensory system:cannot be elicited.
Motor system : Muscle wasting is present , no cramps , no twitching and no involuntary movements
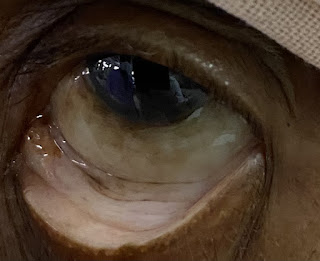
Cranial nerve examination:
1.Olfactory nerve
2.Optic nerve
3.Occulomotor nerve: Normal
4.Trochlear nerve : Normal
5.Trigeminal nerve
Gag reflex present
6. Abducens nerve : normal
8.vestibulocochlear nerve
9. Glossopharyngeal nerve and 10. Vagus nerve- difficulty in speech
11.spinal accesory nerve.
12. Hypoglossal nerve
Tone: Both upper limbs and lower limbs were flexed with increased tone in both flexors and extensors of upper and lower limbs .
Power is 3/5 in upper limbs
Power in lower limbs could not be elicited
Superficial reflexes : Coneal reflex , conjunctival reflex ,abdominal and plantar reflex present .
Deep tendon reflxes
Right
Left
Biceps
+
++
Triceps
+
++
Supinator
+
++
Right
Left
Biceps
+
++
Triceps
+
++
Supinator
+
++
knee jerk reflex could not be elicited.
Babinskis reflex : withdrawal of foot
No signs of meningeal irritation.
Gait could not be assessed .
Glassgow coma scale :
Eye opening - To speech - 4
verbal response - no response - 1
Motor response - Norma flexion - 4
Total - 8
Provisional diagnosis:
Investigations:
TREATMENT:
3% NACL @ 15 ml/ hr
- Head end elevation upto 30 degrees
- Ryles tube feeding
- Ringer lactate
- Normal Saline





















Comments
Post a Comment