A 65 YEAR OLD PATIENT WITH PAIN IN UPPER ABDOMEN
This is an E log book to discuss our patients de identified health data shared after guardians informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency and to comprehend clinical data including history, clinical finding investigations and come up with a diagnosis and treatment plan.
CHEIF COMPLAINTS
- pain in upper abdomen since 3 month
HISTORY OF PRESENTING ILLNESS :
The patient was apparently all right 3 month ago and then he developed pain in the left hypochondriac region and epigastric area which was insidious in onset, gradually progressing, squeezing type, continuous not related to food. The pain was aggravated on inspiration, coughing, and was relieved on lying down on the right side in the fetal position. It does not radiate to other areas.
No H/O fever
No H/O regurgitation, vomiting, malena, hematemesis, nausea
No H/O constipation, burning micturition
PAST HISTORY :
No similar complaints in the past
No previous surgeries in the past
Developed diabetes recently
Not a known case of Hypertension, Epilepsy, tuberculosis, CAD, Asthma
TREATMENT HISTORY
No previous treatment taken
PERSONAL HISTORY:
DIET- mixed
Appetite- reduced
Sleep- normal
Bowel and bladder- normal
Addictions- 250 ml per day since 30 year. Last binge was 3 months ago
40 beedi per day since 50 years. Last one 3 months ago.
GENERAL EXAMINATION:
The patient was conscious, coherent, cooperative. Well oriented to time, place and person.
Moderately built and moderately nourished.
Patient was examined in a well lit room after taking consent.
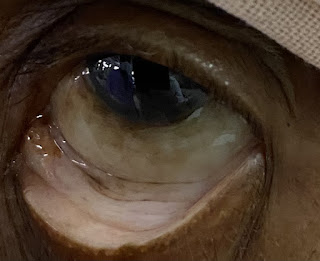
Pallor present
No icterus, cyanosis, clubbing, lymphadenopathy, edema
VITALS:
Temperature- afebrile
BP- 120/80
HR- 82 bpm
RR- 18 cpm
SYSTEMIC EXAMINATION
PER ABDOMEN:
INSPECTION:
Shape of abdomen: Scaphoid
Hyperpigmented rash present on the suprapubic and lumbar region bilaterally.
PALPATION:
Tenderness present in the left hypochondrium and epigastric area.
No guarding, rigidity.
CVS:
S1, S2 heard
RESP:
NVBS, BAE
CNS:
No focal neurological deficits
PROVISIONAL DIAGNOSIS:
Chronic pancreatitis with de novo diabetes
INVESTIGATIONS

















Comments
Post a Comment