A 27 year old patient with fever
Date: November 20th 2022
This is an E log book to discuss our patients de-identified health data shared after guardians informed consent.
here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve this patients clinical problems with collective current best evidence based inputs.
This E-book also reflects my patients centered online learning portfolio and your valuable comments in comment box are most welcome.
I have Been given this case to solve in an attempt to understand the topic of "patient clinical data analysis"to develop my competency and comprehending clinical data including history,clinical finding investigations and come up with a diagnosis and treatment plan.
November 20th 2022
P R C KARTHIKEYA VARMA
ROLL NO:199.
CASE
A 27 year old patient came with chief complaints of:
1. fever since 4 days
2. black coloured stools 1 episode since 1 day.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 4 days ago then developed fever. fever was of high grade, intermittent and there is evening rise of temperature. Patient also had rash on the abdominal area 3 days ago but rash receded as of now. fever is not associated with chills, rigours. Also there is no H/O sore throat, joint pain, burning micturition. no H/O retro-orbital pain.
one episode of malena since yesterday.
PAST HISTORY:
N/K/O diabetes,hypertension,TB, Asthama, CAD,epilepsy.
PERSONAL HISTORY:
appetite: normal.
bowel and bladder movements: regular.
diet: mixed.
sleep: adequate.
NO H/O Addictions.
FAMILY HISTORY:
mother also developed dengue at similar times.
only two of them where living in the house.
not any relavant family history.
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative well oriented to time and place
PALLOR: absent.
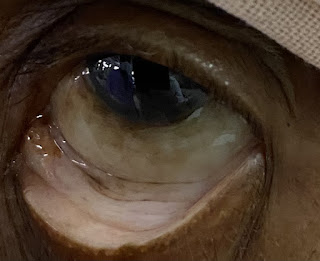
icterus: absent.
cyanosis: absent
clubbing: absent.
lymphedenopathy: absent
edema: absent
VITALS:
temperature: 98c/f
pulse rate: 80
respiratory rate: 18/min
blood pressure: 110/80.
SYSTEMIC EXAMIONATION:
CVS:
cardiac sounds S1,S2 heard.
no thrills, no audible murmurs.
INVESTIGATIONS:
LIVER FUNCTION TESTS
SERUM ELECTROLYTES.








Comments
Post a Comment